November is American Diabetes Month, which is a time to take action together to raise awareness and draw attention to the importance of proper diabetes education. Learn more at www.diabetes.org.
 “You don’t realize how bad your body feels until you change something. I feel so much better now and that was worth it.”
“You don’t realize how bad your body feels until you change something. I feel so much better now and that was worth it.”
When we think about treating diabetes, the first thing that usually comes to mind is insulin injections or staring down a pillbox. But instead of looking into the medicine cabinet, is there a way we can take a glance in our fridge and manage type 2 diabetes? Yes! As the Greek physician, Hippocrates said, “Let food be thy medicine and let medicine be thy food.”
Type 2 diabetes occurs when the body doesn’t respond to insulin. Think of insulin as a key that unlocks the door to let sugar or glucose into your cells. When the key is not working, then the extra glucose floats around in our bloodstream and we get high blood sugar readings.
Why does this happen? Exactly why is unknown, but we do know our genes and lifestyles (including being overweight and/or inactive) influence it. We can’t really mess with our genes. We have to deal with the deck of cards we are dealt, BUT we can control lifestyle choices.
So, the million-dollar question: What is the diet I need to be following to positively affect type 2 diabetes? Is it high fat? Is it low carb? How does the nutrition community feel about keto nowadays?
The answer – and to be honest, you may not like it – isn’t simple and you need to look at what YOUR body says. Doing your research and gathering data is the best way to answer this question. Working on small lifestyle changes can make the body more sensitive to insulin.
Even though it’s the holiday season, there’s no reason to wait to get started. The following strategies can help you start making positive changes NOW:
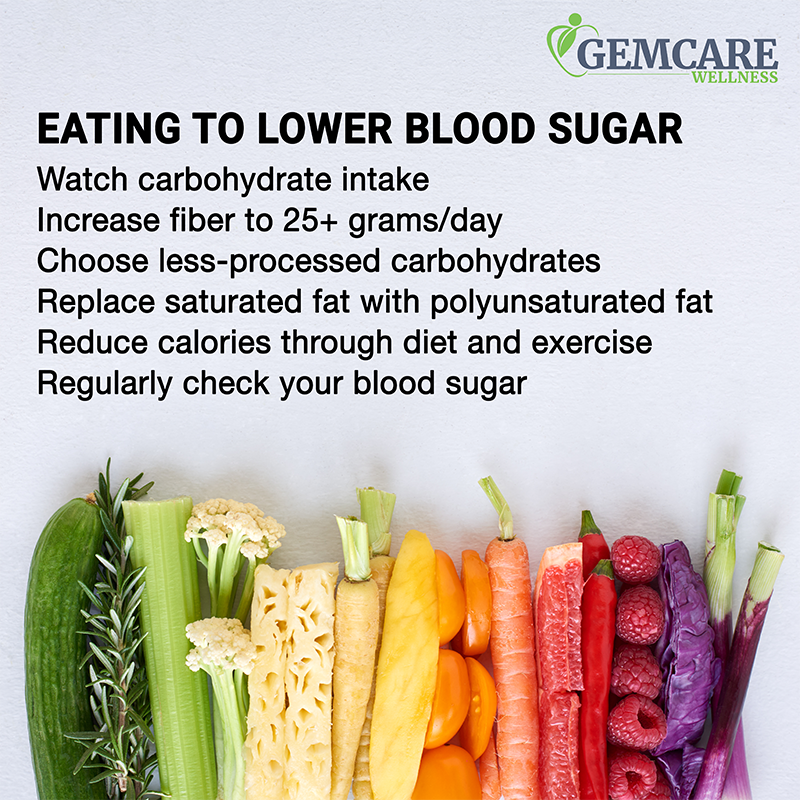
- Watch your carbohydrate intake – there are lots of free apps that can help you track daily intake.
- Increase your fiber to at least 25 grams per day – think leafy greens, broccoli, cauliflower, and beans.
- Choose less-processed carbohydrates over highly processed carbs – an apple a day keeps the doctor a day, not an apple juice box a day!
- When possible replace saturated fats with polyunsaturated fats – think less fat from protein (meat) and more from plants (like avocados).
- Watch how a high-fat meal affects blood sugar – high-fat meals may delay the breakdown of food and blood sugar spike, and also increase insulin requirements.
- Lower your calorie intake, either through food or increasing movement – this helps the body use the glucose better and tends to lower blood sugars.
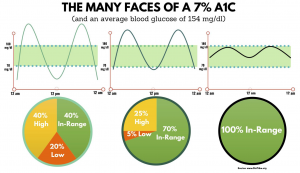
- Regularly check your blood sugar to make sure it is in range and to identify how your diet and exercise impact the numbers.
But what benefit do you get out of focusing on how to eat? Some numbers are lower on a glucose meter, so what? Our clients tell us every day why making good choices is important! One client was diagnosed with type 2 diabetes and started checking his blood sugar per doctor’s orders. He could not seem to get it below 200 mg/dL, which is a high reading. We focused on making small changes like eating smaller portions, eating out one day less in a week, and giving up bread. He recently told us that his blood sugar no longer goes above 140 mg/dL, a reading well within range! He also said, “You know, you don’t realize how bad your body feels until you change something. I feel so much better now and that was worth it.”
Another client really struggled with adjusting his NPH insulin. Because this is a fixed dose of rapid and background insulin, the client must eat the same amount of carbohydrates at around the same time per day. In the summer this was a hard routine to follow. A lot was going on, this client’s weight had gotten to his highest point, and he was taking around 38 units of insulin twice a day. Sometimes at night, he would go so low that he would have to use glucose tabs. With trial and error and working with his Registered Dietitian, he tested what foods worked for him. He decided on a lower-carbohydrate meal pattern. Each day, he planned for 2 proteins, 2 servings of fruit, 3 servings of veggies, and 2 servings of carbs. Through focusing on this lower-carb, balanced approach for three months, he is down 20 pounds and is only using 18 units of insulin a day!
Lifestyle choices allow us to be in charge of type 2 diabetes. Nutrition is a way to feel better, lower blood sugar levels, lose weight, and possibly reduce medication needs. If you’d like extra help with meal planning or have questions related to type 2 diabetes, feel free to reach out to contact us today to set up a consultation!
If you have not been diagnosed with type 2 diabetes, but have prediabetes or are at risk of prediabetes, check out our virtual Diabetes Prevention Programs. These online programs are sponsored by the Ohio Department of Health and free to participants. Classes start in January, so sign up today: https://www.gemcarewellness.com/programs/diabetes-prevention/